What to do If your Health Insurance Claim is Rejected: Health insurance claim rejection is a stressful experience for policyholders, especially when they believe their claims are legitimate. According to a recent study conducted by ET Wealth, 88% of policyholders face issues in claim settlements, and about 69% see their claims either rejected or only partially settled. Navigating the rejection process can be overwhelming, but there are clear steps to follow to address the problem and increase your chances of resolving the issue.
Also see: Best Health Insurance Plans with BP and Diabetes Cover from day one
Understanding Claim Rejections: Common Causes
Before diving into the steps to address a rejected claim, it’s important to understand the common reasons behind claim rejections. Often, rejections occur due to:
- Pre-existing conditions that were not disclosed at the time of buying the policy.
- Incomplete or incorrect documentation, including missing medical records.
- Policy lapse, where the policy was not active at the time of claim.
- Discrepancies in the claim, such as unclear medical conditions during tele-verification.
- Waiting periods not being completed, especially for conditions that require specific timelines.
While some rejections are due to genuine errors or policy exclusions, others can be resolved by understanding and utilizing the right grievance channels.
Also see: Niva Bupa Health Insurance Claim Process in Hindi
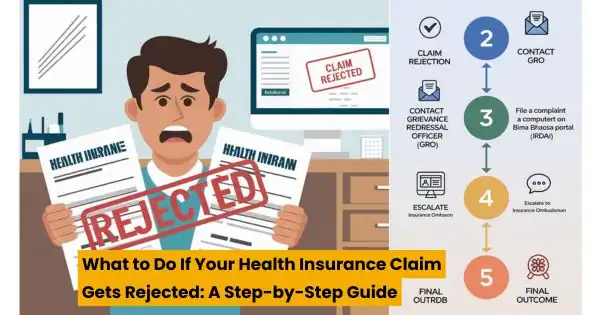
Step 1: Contact the Grievance Redressal Officer of Your Insurance Company
The first action to take after receiving a rejection or partial settlement is to reach out to the Grievance Redressal Officer (GRO) of your insurance company. Every insurer is required to have a Grievance Redressal Mechanism, and the contact details of the GRO can typically be found on the company’s website.
The Grievance Redressal team reviews your case, discusses the matter with the claims department, and provides a resolution. In many cases, this team may identify documentation gaps or procedural issues that can be rectified. It’s vital to have a well-organized file containing all supporting documents, including:
- Policy documents
- Claim submission records
- Correspondence with the insurer
- Medical bills and reports
If the insurer’s response through this channel is unsatisfactory or if you don’t receive a reply within 15 days, you can escalate the matter further.
Step 2: File a Complaint on the Bima Bharosa Portal (IRDAI)
The next step is to file a complaint with the Insurance Regulatory and Development Authority of India (IRDAI) through the Bima Bharosa portal. IRDAI is the regulatory body overseeing insurance companies in India, and the Bima Bharosa portal is their platform for dispute resolution.
Here’s how to file a complaint:
1. Log in to Bima Bharosa Portal: Visit bimabharosa.irdai.gov.in and register your complaint. Ensure you have the following information:
- Policy number
- Detailed description of your grievance
- Supporting documents, such as medical reports, claim letters, and correspondence.
2. Submit the complaint: After completing all sections, upload the necessary files and submit the complaint.
Alternatively, you can email the IRDAI at complaints@irdai.gov.in, providing a complete case history, including:
- The dates of claim submission and rejection.
- Correspondence with the grievance team.
- Any investigation or medical assessments done as part of the claim process.
If you prefer to file a complaint in writing, the postal address of the IRDAI is available on their website. After submitting the complaint, the IRDAI will instruct the insurance company to reassess the case, potentially leading to a revised decision.
Step 3: Escalate to the Insurance Ombudsman
If the resolution provided by the IRDAI does not meet your satisfaction, the next escalation step is the Insurance Ombudsman. The Ombudsman is an independent authority responsible for resolving disputes between policyholders and insurance companies in an impartial manner.
How to File a Complaint with the Insurance Ombudsman
- Visit the Ombudsman’s Website: Go to the Insurance Ombudsman website and register your complaint online. The portal will guide you step-by-step through the process, asking for all relevant details and documents.
- Written Complaint: You can also send a physical complaint to the Ombudsman, including all supporting documents such as policy details, medical reports, and correspondence with the insurer and IRDAI.
- Prepare for a Time-Consuming Process: Resolving a complaint through the Ombudsman can be a lengthy process, sometimes taking several months. The Ombudsman reviews all submitted evidence and may organize meetings between you, the insurance company, and a representative from their office.
A real-life example illustrates the persistence required in this process: A policyholder who ported her health insurance policy from one company to another faced claim rejection for a hernia surgery. The insurer denied the claim, citing undisclosed pre-existing conditions. However, the pre-existing condition had been disclosed in the proposal form, though it was missed during tele-verification. The policyholder contacted the grievance team, but the insurer still rejected the claim. After escalating the matter to the Ombudsman, the case was resolved almost a year later, with the policy reinstated and the claim amount of ₹2.78 lakhs approved.
This case shows that while the process is time-consuming, it can lead to a positive outcome if your claim is genuine and well-documented.
Documents Required for Filing a Complaint
Whether approaching the IRDAI or the Insurance Ombudsman, it is crucial to maintain a detailed and organized set of documents. Here’s what you will need:
- Policy documents: Proof that the policy was active at the time of the claim.
- Claim forms: Copies of the forms submitted to the insurance company.
- Medical records: Reports, prescriptions, and hospital bills related to the claim.
- Correspondence: All emails, letters, and notes from calls with the insurance company.
- Proof of premium payments: Receipts or bank statements showing that premiums were paid on time.
- Proposal form: In cases involving pre-existing conditions, the original proposal form where details were disclosed.
Follow-Up and Persistence
Filing a complaint with the IRDAI or the Insurance Ombudsman is not a quick fix. Be prepared for multiple rounds of correspondence, and keep detailed records of every communication. In the case mentioned earlier, the policyholder had to follow up for nearly a year, including attending online meetings with representatives of the insurance company and the Ombudsman’s office.
Outcomes: What Can You Expect?
There are three possible outcomes when filing a grievance:
- Claim settlement: If the grievance is found to be valid, the insurance company will be instructed to settle the claim.
- Rejection upheld: If the insurer proves that the claim was denied based on valid policy exclusions, the Ombudsman or IRDAI may uphold the rejection.
- Policy reinstatement: In some cases, the insurer may reinstate a terminated policy if the grievance is resolved in the policyholder’s favor.
Conclusion
Rejection of claims is common these days, but policyholders have several avenues for redressal. From the insurance company’s grievance redressal officer to IRDAI and the Insurance Ombudsman, there are structured processes to address legitimate complaints. The key to success is persistence, detailed documentation, and a full understanding of your policy terms. If your claim is valid, these steps can help you get the compensation you deserve and ensure that the insurer follows the guidelines set by regulatory authorities.
FAQs about What to do If your Health Insurance Claim is Rejected
What should I do if my health insurance claim is rejected?
Start by contacting the Grievance Redressal Officer (GRO) of your insurance company. If you’re not satisfied with their response, escalate the issue by filing a complaint with the IRDAI through the Bima Bharosa portal.
How long does it take to resolve a rejected claim?
The resolution process can be lengthy, especially if escalated to the Insurance Ombudsman. It may take several months, with some cases taking up to a year for a final resolution.
What documents do I need to file a complaint with IRDAI or the Ombudsman?
Key documents include your policy papers, claim forms, medical records, correspondence with the insurer, proof of premium payments, and any other supporting documentation related to the claim.
Can the Insurance Ombudsman overturn a claim rejection?
Yes, if the Ombudsman finds the claim rejection to be unjustified, they can instruct the insurance company to settle the claim and even reinstate a lapsed policy.
Is there a time limit to file a complaint after my claim is rejected?
Yes, it’s important to file a complaint within the stipulated timeframe as outlined by the insurance company and IRDAI, typically within a few months of the rejection.
Disclaimer: The information provided in this article is for general informational purposes only and does not constitute professional legal or financial advice. While every effort has been made to ensure accuracy, insurance policies and claim procedures may vary. Readers are advised to consult their insurance provider or a legal expert for specific guidance regarding their individual claims or grievances.

If health insurance, Life insurance and any other insurance climes are rejected on simple reasons, please contact for legal guide lines –
D.Srihari Advocate/ Insurance Advoicer
Cell; 9440386026
Place:- Nirmal dist of (T.S)